Dawn of Next Generation IOP in Delray Beach
Coastal recovery environment benefits
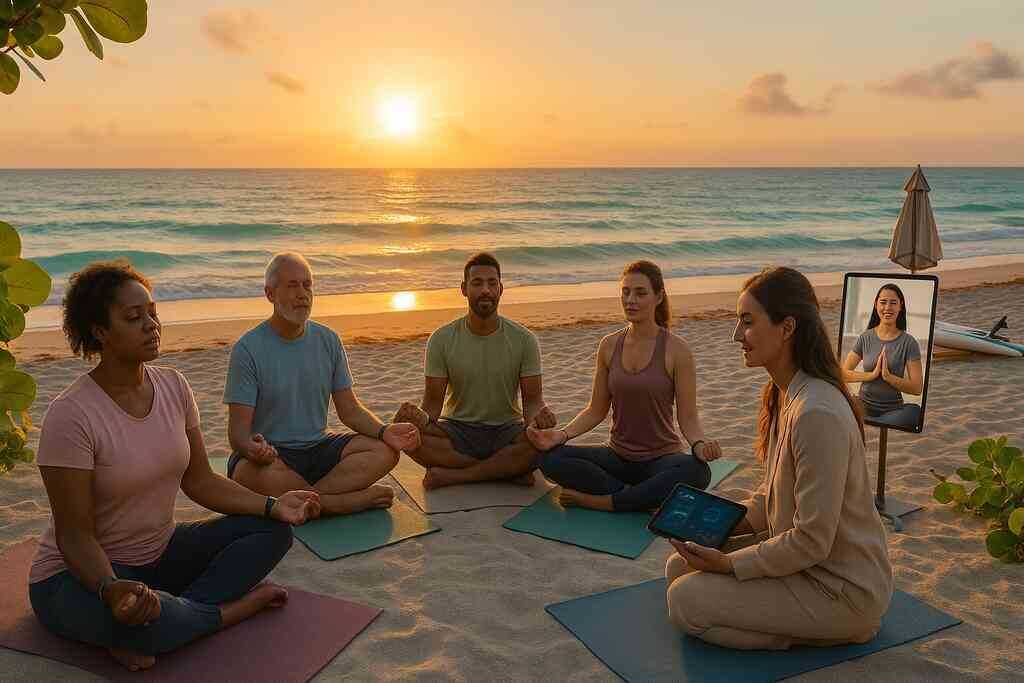
Ocean air, warm breezes, and year-round sunshine deliver a healing backdrop that science now calls blue-mind therapy. Research shows coastal settings lower cortisol, improve sleep, and boost motivation, making them ideal for sustainable alcohol recovery. Against that scenic canvas, our premier outpatient recovery on Delray Beach leverages the ocean’s restorative effects to elevate therapy. Clients in intensive outpatient programs near you practice mindfulness while seabirds glide overhead, translating coping skills into immediate sensory experience. Because emotional regulation begins with felt safety, the shoreline becomes an evidence-infused classroom where stress dissolves and hope flows.
Location matters in rehabilitation centers, and Delray Beach’s proximity to ocean and vibrant amenities offers a rare dual advantage. Morning group therapy may unfold beneath a pergola scented by sea grapes. Afternoon clinical work occurs inside climate-controlled treatment centers outfitted with advanced biofeedback. Moreover, accessibility matters; clients seeking an IOP near you fly into nearby airports and reach sessions quickly. Convenience marries beauty, reinforcing attendance and strengthening recovery programs without compromise.
The catalyst for evidence based rehab evolution
Delray Beach IOP clinicians continuously scan peer-reviewed journals, integrating breakthroughs the moment efficacy is proven. Cognitive behavioral therapy merges with mindfulness-oriented recovery enhancement, producing blended protocols that outperform traditional stand-alone sessions. Pharmacogenetic testing now informs medication management, letting physicians personalize dosages and avoid side effects that sabotage engagement. Because these intensive outpatient programs in Delray Beach measure outcomes weekly, data feedback loops spotlight interventions that truly reduce cravings. The result is an ever-evolving treatment matrix where science, compassion, and real-time analytics converge to accelerate brain-body healing.
Artificial intelligence now acts as a silent teammate, flagging mood shifts before relapse risk peaks. Wearable sensors transmit heart-rate variability to clinicians, who adjust coping assignments through secure portals. These predictive models transform ordinary rehab services into proactive safeguards that meet cravings at the door. Patients feel empowered because feedback arrives as encouraging nudges on their phones rather than reprimands in group. Momentum builds, and evidence-based rehab evolution gains unstoppable force within every session.
Why the Delray Beach wellness ecosystem matters
Treatment never happens in a vacuum, and the local wellness ecosystem amplifies gains earned in therapy. Delray Beach hosts an impressive cluster of wellness centers, mental health facilities, detox facilities, and sober-living residences within walking distance. This density lets clients transition from detox to IOP continuity without delays that often erode motivation. Collaborative agreements among Florida rehab centers streamline referrals, ensuring that nutritional counseling, chiropractic care, and trauma-informed yoga complement core psychotherapy. When every provider speaks a shared language of evidence and empathy, sustainable change becomes the community default.
Community also extends to culture, and Delray’s art walks, farmers’ markets, and peer-led beach cleanups offer sober social laboratories. These activities reinforce purpose while exposing participants to role models who thrive in long-term recovery. By weaving healthy routines into local traditions, intensive outpatient programs create neural associations between joy and sobriety. Families visiting for weekend sessions witness these vibrant scenes and finally envision a future beyond crisis. Hope spreads outward, proving that the Delray Beach wellness ecosystem is not simply supportive-it is transformative.
Personalized Pathways: Powered by Neuroscience and Digital Therapeutics
AI guided therapy sessions and adaptive care plans
Artificial intelligence now personalizes every session before a counselor greets the client. Algorithms scan assessments, past notes, and biometric patterns to recommend micro-interventions within personalized intensive outpatient models. Clinicians inside our next gen intensive outpatient programs in Delray anchor therapy decisions to those insights. The resulting care plan updates each week, mirroring the patient’s shifting triggers. Because data guides decisions, wasted sessions vanish and motivation rises.
Adaptive software flags rising stress before cravings surface. Counselors receive alerts, allowing them to adjust coping skill drills on the fly. Patients view the process through dashboards that translate scores into plain language, fostering ownership. Transparency reduces anxiety because surprises disappear and progress feels measurable. Such AI-guided therapy turns abstract neuroscience into practical, daily victories. These innovations illustrate the future of Delray Beach IOP where technology and empathy merge seamlessly.
Wearable monitoring in recovery and real time data loops
Wrist sensors, smart rings, and pocket ECG devices now join the therapeutic team. These digital therapeutics for recovery transform passive wearables into active guardians. They capture sleep, heart-rate variability, and micro-tremors that often predict relapse hours ahead. Clinicians contextualize those signals against the scientific overview of intensive outpatient care models, ensuring interpretation stays evidence-driven. When metrics cross a personalized threshold, the platform sends calming breath exercises directly to the client’s phone.
Data also empowers families by sharing summary reports during weekly check-ins. Loved ones view graphical trends instead of vague anecdotes, promoting constructive dialogue. Meanwhile, therapists refine session agendas based on objective physiology, not guesswork. This precision reduces false alarms and prevents compassionate fatigue inside the support network. Over time, small bio-based adjustments yield big reductions in emergency detox returns.
Hybrid telehealth IOP services enhancing access
Not every breakthrough requires a clinic visit, and hybrid telehealth bridges that gap gracefully. These innovative IOP pathways ensure continuity between settings without sacrificing accountability. Video group therapy runs alongside in-person circles, allowing snowbirds to stay engaged while traveling. Cloud platforms integrate securely with electronic health records, so clinicians update notes in real time. Patients appreciate the flexibility because work obligations no longer collide with essential recovery programs. Hybrid delivery therefore increases attendance rates without compromising therapeutic intensity.
Counselors tailor the mix of digital and on-site hours based on acuity, resources, and learning style. For rural Floridians, telehealth becomes a lifeline by eliminating long drives and childcare hurdles. For urban professionals, lunchtime check-ins replace stressful commutes through traffic. Either way, accessibility fuels momentum, which remains the single greatest predictor of sustained change. With obstacles minimized, clients devote energy to mastering neuroscience-based skills rather than logistics.
Neuroscience driven treatment plans in intensive outpatient programs
Modern brain imaging shows addiction rewires neural circuits responsible for motivation, memory, and decision-making. Delray Beach IOP clinicians translate these findings into concrete exercises that rebuild healthy pathways. For example, cue-exposure therapy pairs beachside breathing drills with controlled trigger visualization, retraining amygdala responses. Repetition under safe conditions dampens the fight-or-flight impulse and strengthens prefrontal regulation. Each client’s protocol evolves as neural metrics improve, ensuring stimulation never becomes stagnant.
Pharmacogenomic testing complements brain-based therapies by identifying medications that align with each client’s metabolic profile. Side effects drop, adherence climbs, and trust deepens when bodies respond predictably. Nutritional neuroscience also enters the plan, with omega-3 supplements and gut-brain diet coaching supporting plasticity. Because evidence drives every choice, program outcomes feed a growing database that powers future refinements. The cycle of measurement and adaptation ensures Delray Beach continues leading innovative IOP pathways nationwide.

Integrating Mental Health: Wellness and Community Reintegration
Trauma informed outpatient care across Florida rehab centers
Trauma histories often drive substance use, so every intensive outpatient program must acknowledge that reality first. Our clinicians adopt the sanctuary model, ensuring sessions remain physically, emotionally, and culturally safe. That commitment grows stronger through collaboration with neighboring Florida rehabilitation centers and detox facilities. Together, we coordinate referrals and share training resources, strengthening integrated mental health therapy near Palm Beach. Consequently, patients move from crisis detox to nurturing IOP in Delray Beach without losing momentum.
Trauma-informed language also permeates group rules, replacing judgment with curiosity. Therapists invite each participant to control lighting, seating, and pacing, reinforcing autonomy. Moreover, somatic techniques like bilateral tapping reduce hyperarousal before narratives emerge. Because the brain processes danger subconsciously, these grounding rituals keep prefrontal regions online during disclosure. As safety grows, clients tolerate deeper work, accelerating breakthroughs that previously stalled in traditional recovery programs.
Holistic alcohol recovery programs and mindfulness practice
Holistic alcohol recovery programs view sobriety as more than abstinence; they nurture mind, body, and spirit simultaneously. Delray Beach IOP harnesses coastal geography to facilitate sunrise meditation, paddleboard yoga, and mindful walking. These embodied exercises recalibrate the vagus nerve, which governs emotional regulation and craving suppression. Meanwhile, nutritionists teach anti-inflammatory meal planning, reinforcing neuroplasticity with gut-brain synergy. Such integrative layers convert scenic beaches into living laboratories where evidence-based rehab evolution feels tangible.
Clients also receive personalized breathwork playlists delivered through mobile apps developed by our digital therapeutics team. The platform adjusts tempo based on real-time heart-rate variability collected during sessions. Consequently, mindfulness practice continues after appointments, guarding evenings when relapse risk secretly rises. Over weeks, biometric feedback proves progress, inspiring adherence among those skeptical of abstract meditation promises. Most importantly, holistic routines lower anxiety without medication, allowing physicians to prescribe judiciously.
Family inclusive rehab strategies for resilient homes
Addiction strains entire households, so family inclusion remains a pillar within intensive outpatient programs near you. Facilitators use structured dialogue models that equalize speaking time and prevent blame spirals. They also teach attachment-based parenting skills, enabling caregivers to replace control with connection. As relationships stabilize, relapse triggers diminish because environmental stress cues become supportive reminders instead. Ultimately, resilient homes extend therapeutic gains far beyond clinic hours, strengthening the Delray Beach wellness ecosystem.
Virtual participation options ensure distant relatives join weekly workshops without disrupting work responsibilities. Furthermore, clinicians supply recorded psychoeducation modules translated into multiple languages for multilingual households. Transparency about insurance-friendly treatment options alleviates financial tension that otherwise erodes solidarity. When everyone understands cost, trajectory, and expected hurdles, unified commitment replaces uncertainty. This clarity echoes value-based behavioral health principles, driving accountability at every stage.
Peer led support networks and community reintegration pathways
Nothing reinforces change like walking beside someone who has survived the same storm. Therefore, Delray Beach Intensive Outpatient Programs cultivates peer mentors who co-facilitate skill groups. Their lived experience normalizes setbacks and models practical problem-solving in real time. Moreover, mentors accompany clients to volunteer events, art nights, and beach cleanups, bridging clinic and community. That exposure de-stigmatizes recovery, transforming Delray Beach into a tapestry of hopeful narratives.
Many graduates strengthen accountability through peer support via Alcoholics Anonymous meetings. IOP clinicians coordinate with local chapters to align discussion themes with weekly therapy objectives. Consequently, vocabulary, milestones, and slogans remain consistent, minimizing confusion during vulnerable moments. As social circles expand, employment networking and recreational plans emerge organically, supporting community reintegration pathways. Peers celebrate milestones publicly, replacing isolation with collective pride and forward momentum.
Culturally competent care models for diverse populations
Delray Beach attracts residents and visitors from countless cultural backgrounds, each carrying unique recovery expectations. Culturally competent care therefore becomes essential, not optional, within our intensive outpatient programs in Delray Beach. Assessments now include questions about spiritual beliefs, family hierarchy, and preferred healing rituals. Therapists use that information to adapt metaphors, homework, and group pairings without diluting clinical integrity. Such nuanced adjustments increase trust, which directly predicts retention and long-term sobriety.
Language access services provide professional interpreters rather than relying on family members to translate sensitive content. Additionally, culinary therapy menu planning respects halal, vegan, or allergen-free preferences during nutritional workshops. Group facilitators also honor holidays from different faiths, adjusting schedules so participants never choose between recovery and tradition. When individuals feel seen, attendance improves and community ambassadors willingly recommend programs to friends. Delray’s influence on upcoming IOP care therefore grows organically, fueled by culturally aligned success stories.
Measuring Success With Value Based Outcome Metrics
Outcome measurement in rehab and continuous improvement
Outcome data fuels every innovative IOP pathway, yet numbers only matter when they guide meaningful change. Clinicians at Delray Beach Intensive Outpatient Programs gather standardized scales on craving intensity, mood stability, and functional capacity at the start of each week. They compare individual progress against the broader overview of intensive outpatient care models to ensure benchmarks remain evidence-aligned. When a score trends down, therapists refine interventions immediately, preventing small slips from snowballing into relapse. This continuous-improvement loop converts abstract statistics into personalized victories, reinforcing trust between clients and their multidisciplinary team.
Real-time dashboards visualize those metrics on large clinic monitors, turning therapy halls into transparent learning labs. Staff huddle every morning to celebrate gains and troubleshoot gaps, applying agile principles long used in top technology firms. That culture shift produces an atmosphere where feedback feels empowering, not punitive, which energizes every recovery program. Because insights update hourly, outdated protocols disappear quickly and fresh techniques surface faster. Such responsiveness reflects the pioneering care strategies at Delray IOP that position the center as a model for nationwide adoption.
Value based behavioral health financing and insurance friendly models
Payers now reward quality over quantity, so Delray Beach IOP aligns its financial model with measurable health improvements. The team maps each treatment episode against cost, engagement, and long-term sobriety, proving that outcomes justify reimbursement. This data-driven transparency makes the program highly attractive to carriers seeking reduced readmission expenses. Clients benefit because the streamlined admissions process for IOP eliminates paperwork bottlenecks, accelerating entry into care when motivation peaks. Ultimately, value-based financing shifts the conversation from price to performance, removing hidden fees and clarifying every dollar’s purpose.
Bundled-payment pilots further integrate detox, IOP sessions, and aftercare coaching into one predictable package. Insurers know exactly what they fund, while families avoid cascading invoices that increase stress. Moreover, performance bonuses encourage clinicians to share best practices across Florida rehab centers, lifting statewide standards. Data analytics highlight which modalities deliver the highest return, making budgeting both ethical and strategic. By linking dollars to documented gains, Delray Beach sets a precedent for modern, insurance-friendly treatment centers everywhere.
Accredited treatment centers excellence and safety standards
Excellence requires accountability, so Delray Beach Intensive Outpatient Programs maintains more than thirty accreditations from industry watchdogs. These external reviews test client safety procedures, medication storage, and ethical billing, ensuring no corner gets cut when pressure rises. Auditors also verify culturally competent protocols, confirming that diverse populations receive equitable care. Families researching options can explore the extensive credentials listed on the about the Delray Beach IOP ecosystem page and feel instant reassurance. Accreditation therefore functions as both shield and spotlight, guarding clients while showcasing best-in-class performance.
Safety metrics do not sit idle after the certificates arrive; they feed monthly quality-improvement meetings. Staff analyze incident-report patterns and near-miss logs to identify hidden vulnerabilities before harm occurs. Electronic health-record alerts flag potential medication interactions, while routine simulation drills sharpen crisis response. This rigorous environment cultivates a mindset where every employee becomes a guardian of excellence. In turn, patients experience consistent, predictable care that accelerates mental health integration within IOP frameworks.
Relapse prevention technology and detox to IOP continuity
Seamless transitions guard recovery momentum, so Delray Beach IOP pairs biometric wearables with mobile apps that predict risk hours before cravings bloom. This proactive stance represents the future focused recovery techniques for 2026 already practiced daily at the facility. When heart-rate variability drops, the system sends calming exercises and notifies the therapist, who can schedule an urgent video session. These timely interventions reduce emergency detox returns and keep clients engaged in their personalized intensive outpatient model. Technology thus evolves from simple monitoring to an active therapeutic ally.
Continuity also relies on level-of-care flexibility, enabling clients to step down gradually rather than face an abrupt exit. Medical directors coordinate with the in-house detox unit and with trusted partial hospitalization options in Delray Beach to create smooth handoffs. Shared electronic records ensure no story gets lost between providers, preserving therapeutic rapport. Additionally, peer mentors accompany clients during transition visits, demystifying new environments and reinforcing coping skills. This integrated pathway safeguards steady progress, proving that relapse prevention begins the moment detox starts, not after discharge.
Navigating the Horizon of Sustainable Recovery
Sustainable sobriety coaching and resilience training workshops
Sustainable sobriety coaching turns abstract recovery ideals into daily rituals that last. Certified coaches meet clients after standard sessions, translating neuroscience-driven treatment plans into bite-sized goals. They track progress with wearable monitoring in recovery dashboards, celebrating micro-wins to reinforce neural reward circuits. Because every milestone is visible, motivation compounds and relapse prevention technology feels empowering rather than invasive. Over time, personalized intensive outpatient models mature into lifelong playbooks that work anywhere-not just in a therapy room.
Resilience training workshops complement coaching by teaching stress inoculation skills in dynamic group formats. Participants rehearse pressure scenarios drawn from real life, then debrief using CBT and mindfulness. The process strengthens prefrontal regulation while normalizing vulnerability through peer-led support networks. Workshops also weave in holistic alcohol recovery programs such as breath-work and functional fitness, proving wellness can be both rigorous and fun. Clients leave each session with concrete tools instead of vague inspiration.
Co creating the future of Delray Beach IOP with patient centered care
True innovation blossoms when patients guide program design rather than merely receiving it. Delray Beach IOP staff host quarterly co-creation forums where alumni, families, and clinicians brainstorm next-generation IOP in Delray Beach features. Ideas then enter agile development sprints, mirroring best practices from Florida rehab centers innovation labs. One recent forum produced a mobile mood-mapping tool that syncs with AI-guided therapy sessions, closing feedback loops between visits. This iterative culture ensures evidence-based rehab evolution never stalls.
Financial transparency also powers collaboration, linking value-based behavioral health metrics to individualized goals. Clients learn how outcome measurement in rehab influences insurance-friendly treatment options, fostering shared accountability. When everyone understands the scorecard, trust deepens and engagement rises sharply. Such patient-centered care pathways demonstrate that healing thrives where voices matter and data serves people, not the other way around.
Embracing community resilience for lifelong recovery
Delray Beach’s shoreline, art scene, and volunteer culture create fertile ground for community reintegration pathways. Clients practice new skills during beach cleanups, farmers’ markets, and charity races, converting coastal recovery environment benefits into lived experience. These public victories erode stigma while showcasing the Delray Beach wellness ecosystem as a partner in healing, not just a backdrop. Graduates often return as mentors, proving sustainable change is contagious.
Strategic initiatives extend beyond local borders through coordinated outreach and digital therapeutics for recovery. The center’s 2026 roadmap for Delray Beach IOP evolution outlines regional alliances, telehealth expansions, and culturally competent care models that respect every voice. By integrating trauma-informed outpatient care with hybrid telehealth IOP services, the program safeguards detox-to-IOP continuity even when life gets complicated. As resilience training workshops multiply, the future of Delray Beach IOP looks less like a clinic and more like a thriving, interconnected community devoted to lifelong recovery.
Frequently Asked Questions
Question: How will AI-guided therapy sessions enhance personalized intensive outpatient models at Delray Beach IOP by 2026?
Answer: Artificial intelligence already scans each client’s assessments, biometric trends, and session notes to shape a totally individualized plan before the first appointment begins. By 2026 these AI-guided therapy sessions will integrate real-time data from wearable monitoring in recovery, instantly adjusting coping drills or medication schedules when stress indicators spike. This evidence-based rehab evolution means fewer wasted sessions, faster progress, and a treatment experience that feels as unique as the person receiving it. Clients can expect micro-interventions delivered through secure apps, while our clinicians harness predictive analytics to keep relapse risk low-making Delray Beach Intensive Outpatient Programs the gold standard for personalized intensive outpatient models in Florida.
Question: What role will wearable monitoring in recovery play in the relapse-prevention technology offered by Delray Beach Intensive Outpatient Programs?
Answer: Smart rings, ECG patches, and wrist sensors will act as 24/7 guardians that feed heart-rate variability, sleep quality, and stress markers directly into our clinical dashboards. When algorithms detect patterns that historically precede cravings, clients receive calming breathwork videos while therapists are alerted to schedule an immediate check-in-often long before a lapse occurs. This seamless detox-to-IOP continuity transforms relapse prevention technology from reactive to proactive, strengthening every phase of our intensive outpatient programs in Delray Beach and reinforcing the broader Delray Beach wellness ecosystem.
Question: In the blog title What Is the Future of IOP Pathways in Delray Beach by 2026?, you highlight hybrid telehealth IOP services-how will these improve access to intensive outpatient programs near you?
Answer: Hybrid telehealth IOP services combine the best of on-site coastal recovery environment benefits with secure video sessions that travel wherever clients do. Snowbirds can join group therapy from up north, busy professionals can attend lunchtime CBT modules from the office, and rural Floridians avoid long drives to Florida rehab centers altogether. All telehealth sessions sync automatically with our electronic health records, keeping AI-guided therapy recommendations current. The result is higher attendance, lower dropout rates, and truly accessible intensive outpatient programs near you without sacrificing the clinical rigor Delray Beach IOP is known for.
Question: How do trauma-informed outpatient care and culturally competent care models integrate into the next-generation IOP in Delray Beach?
Answer: Trauma-informed outpatient care means every group rule, room setup, and therapy exercise is designed for physical and emotional safety. Somatic grounding, bilateral tapping, and choice-based seating empower clients who have survived complex trauma. At the same time, culturally competent care models ensure language access, respect for spiritual practices, and menu options that honor dietary traditions. By weaving these pillars into daily programming, Delray Beach Intensive Outpatient Programs creates an inclusive environment where diverse populations feel seen and supported-accelerating mental health integration in IOP and boosting long-term recovery outcomes.
Question: How does Delray Beach IOP measure success within its value-based behavioral health approach and insurance-friendly treatment options?
Answer: We collect standardized outcome metrics-craving intensity, mood stability, attendance, and functional capacity-at the start of every week. Real-time dashboards compare individual progress against national benchmarks for intensive outpatient programs, allowing clinicians to fine-tune interventions immediately. This data-driven transparency not only fuels continuous improvement but also aligns perfectly with value-based behavioral health contracts, giving insurers clear evidence of cost-effective care. Families appreciate predictable, bundled pricing that covers detox facilities, rehab services, and aftercare coaching, while clients thrive under a model that rewards measurable success. Accredited treatment centers excellence meets insurance-friendly treatment options-all under one Delray Beach shoreline.
