Awakening to Restful Recovery at Delray Beach IOP
The missing pillar in intensive outpatient programs
Sleep seldom headlines treatment plans, yet it fuels every waking recovery victory. Many intensive outpatient programs focus on groups, medication, and relapse prevention, but overlook nightly restoration. At our facility, clinicians view healthy slumber as a clinical vital sign, essential for neurochemical rebalancing. Through tailored sleep hygiene in intensive outpatient programs, patients learn to rebuild circadian rhythms broken by substance use. This philosophy powers the premier Delray IOP restorative sleep support, merging science and compassion for seamless day-therapy and night renewal.
Sleeplessness often persists long after detox, undermining cognition, mood, and decision making. Our clinicians start every admission with a detailed sleep assessment, mapping bedtime routines, nightmare frequency, and chronotype. This data shapes individualized schedules that synchronize therapy sessions with natural energy peaks, maximizing engagement. Clients then experiment with restorative rest strategies for recovery, tracking progress in digital journals reviewed weekly. These gains showcase intensive outpatient sleep therapy solutions in Delray Beach, blending cognitive, behavioral, and environmental tweaks for lasting change.
Linking alcohol recovery success to restorative rest
Alcohol disrupts REM cycles, decreases slow-wave sleep, and leaves the brain starved for nightly repair. Cravings spike when fatigue lowers executive control, turning minor triggers into high-risk moments. Our delray beach IOP sleep therapy protocol teaches clients how quality rest buffers those vulnerabilities, supporting stronger impulse management. Counselors weave psychoeducation into group discussions, illustrating charts that link poor sleep with relapse statistics. Clients explore the mental health and sleep synergy at Delray IOP, seeing mood stability and sound sleep strengthen each other.
During early sobriety, many people misinterpret insomnia as a personal failing rather than a predictable neurochemical rebound. Our therapists normalize these disturbances, explaining how GABA receptors recalibrate and melatonin production gradually returns. Patients practice breathing exercises that calm nighttime cravings, replacing late-night scrolling with mindful body scans. If sleep still feels elusive, medical providers adjust non-habit-forming supplements or recommend brief pharmacological bridges. Our easy admissions for sleep-focused recovery in Florida streamline entry so weary minds get expert help before exhaustion erodes motivation.
How Florida rehab centers are redefining sleep support
Florida’s temperate climate allows recovery plans to leverage natural light exposure, ocean aerosols, and outdoor movement year-round. Delray clinicians schedule sunrise walks that trigger serotonin release, priming the evening melatonin cascade. Evening programs happen just before dusk, letting patients transition directly into mindfulness bedtime rituals at Delray Beach. Bedrooms feature supportive bedding environments, blackout curtains, and white noise options to block campus activity. These details showcase the innovative IOP practices enhancing bedtime healing, inspiring Florida rehab centers to expand sleep-centric amenities.
Research shows patients who achieve seven consecutive nights of quality sleep report higher therapy retention and lower craving intensity. Therefore, our interdisciplinary teams include board-certified sleep medicine consultants alongside addiction psychiatrists and wellness coaches. Together they create circadian rhythm reset schedules, aligning medication dosing, meal times, and exercise with each client’s chronotype. Progress is reviewed through wearable data, giving tangible proof that behavioral sleep interventions in rehab yield rapid cognitive gains. Such coordination defines our comprehensive treatment plans balancing nighttime recovery, showing every Florida IOP can treat sleep as foundational medicine.
The Science of Slumber in Substance Healing
Circadian rhythm reset during IOP treatment
Delray Beach IOP clinicians view the circadian clock as the metronome of recovery, guiding metabolism, mood, and craving resistance. Substance abuse often drags that clock hours off beat, so patients wake groggy and attend therapy half-alert. During intensive outpatient programs in Delray Beach, staff prescribe sunrise exposure, scheduled meals, and consistent lights-out to re-entrain internal timekeepers. Wearable devices capture nightly data, revealing how regular bedtimes align with fewer afternoon dips and steadier emotional regulation. As clients witness tangible progress, motivation soars and engagement deepens.
Providers also adjust group schedules to each participant’s chronotype whenever possible, proving personalized medicine boosts adherence. Early birds complete processing groups before noon, while natural night owls reserve analytic work for late afternoon when cognition peaks. This flexibility demonstrates our commitment to whole-person care rather than one-size-fits-all programming. Many graduates credit their newfound morning clarity to these circadian adaptations, calling the routine a hidden superpower. Seamlessly, healthy sleep transforms therapy from a chore into a catalyst for lasting change through our transformative outpatient recovery and healthy sleep approach.
Neuroplasticity and overnight memory reconsolidation
Every counseling breakthrough requires the brain to file new memories, prune old pathways, and strengthen adaptive circuits. Those tasks peak during slow-wave and REM sleep, when neuroplasticity surges and emotional archives reorganize. Intensive outpatient programs near you that ignore sleep inadvertently sabotage this neurological housekeeping. At Delray Beach, clinicians explain that sober brains need extra consolidation time because early recovery floods neural networks with novel coping skills. Clients therefore treat bedtime like an extension of the therapy day, protecting those hours with the same respect they give group sharing rules.
Regular deep sleep amplifies the benefits of cognitive behavioral therapy by embedding fresh beliefs into long-term storage. Studies show people recalling session insights more clearly after seven quality nights compared to two. Counselors harness that evidence, asking clients to journal positive lessons before bed so the hippocampus can replay them during REM. Over weeks, cravings fade as adaptive pathways dominate. By combining delray beach IOP sleep therapy with neuropsychology education, we turn abstract science into lived experience clients can feel each dawn.
Trauma informed sleep coaching for dual diagnosis clients
Many individuals arrive with both substance use disorder and lingering trauma that fuels hyper-arousal. Nighttime silence can trigger flashbacks, leaving the nervous system too vigilant for rest. Our trauma-informed clinicians introduce grounding techniques, weighted blankets, and secure bedroom layouts to signal safety. Parallel EMDR sessions unpack traumatic memories, decreasing nocturnal startle responses over time. This dual approach reinforces that mental health facilities must weave psychological and physiological tactics together.
Counselors also teach clients to reframe nightmares as messages, not failures. By reviewing distressing dreams in morning sessions, patients reduce shame and discover patterns that guide therapy goals. Gentle yoga nidra, guided imagery, and progressive muscle relaxation give bodies a script for shifting from fight-or-flight into parasympathetic calm. Because dual diagnosis patients often blame themselves for insomnia, staff emphasize how trauma physiology, not weakness, drives midnight wake-ups. That compassion fosters trust, allowing deeper exploration of core wounds while restorative rest strategies for recovery take root.
Insomnia relief strategies during alcohol detox
Alcohol recovery poses unique challenges because the substance initially sedates yet ultimately fragments sleep architecture. As detox begins, REM rebounds ferociously, causing vivid dreams, sweats, and mood swings. Medical teams at our IOP in Delray Beach forecast these symptoms so clients feel prepared rather than panicked. Non-addictive supplements, evening protein snacks, and timed magnesium help smooth neurotransmitter fluctuations. Breathing exercises that calm nighttime cravings replace the old “nightcap” ritual, reinforcing self-efficacy.
Moreover, staff collaborate with nearby detox facilities to synchronize medication schedules with circadian goals, preventing stimulant doses from spilling into bedtime. Clients track hours asleep on digital charts, celebrating even ten-minute gains because small wins matter early on. Peer groups discuss AA meetings near you for sober evenings, offering structure that limits late-night isolation-a frequent insomnia trigger. Over weeks, CBT-I for substance recovery dismantles maladaptive sleep thoughts, proving scientifically grounded behavioral sleep interventions in rehab accelerate healing. Ultimately, restful nights become both a milestone and a shield against relapse.
Evidence Based Sleep Interventions in Our Intensive Outpatient Programs
Personalized sleep assessments and chronotype mapping
Clinicians begin every intake with a comprehensive sleep assessment that rivals any overnight lab, yet feels supportive, not clinical. Patients share bedtime routines, nightmare frequency, and caffeine use while staff record chronotype indicators. These data guide individualized schedules within our delray beach IOP, aligning therapy blocks with natural energy peaks. Consequently, sleep hygiene in intensive outpatient programs stops feeling generic and starts feeling tailor-made. Over subsequent weeks, restorative rest strategies for recovery are refined, and patients witness objective gains through wearable metrics.
Equally important, counselors translate graphs into relatable insights so clients grasp the “why” behind each adjustment. When an early bird sees cravings drop after earlier dinners, motivation soars. Night owls appreciate later group discussions that match their cognitive highs. This adaptive approach illustrates behavioral sleep interventions in rehab that respect diversity rather than enforcing a rigid curfew. Ultimately, personalized mapping becomes a cornerstone of sustained resilience beyond discharge.
CBT-I integration for substance use disorder
Cognitive Behavioral Therapy for Insomnia remains the gold standard, and our IOP in Delray Beach embeds it seamlessly alongside relapse prevention. Therapists dismantle unhelpful sleep beliefs such as “I will never rest sober,” replacing them with data-driven expectations. Clients practice stimulus control techniques, leaving beds when wakefulness exceeds fifteen minutes, then returning only when drowsy. Such structure re-trains the brain to pair pillows with power-down, not frustration. Over several sessions, CBT-I for substance recovery lowers hyper-arousal and sharpens daytime focus.
Moreover, homework assignments anchor progress between meetings. Participants track thoughts and behaviors in concise diaries, identifying triggers like late-night worries about alcohol recovery challenges. Counselors celebrate small improvements, reinforcing self-efficacy and strengthening neural pathways of success. Because sessions occur within intensive outpatient programs in Delray Beach, skills transfer directly to home bedrooms each evening. This immediate real-world application accelerates gains compared to inpatient settings where environmental control differs.
Guided meditation and progressive muscle relaxation sessions
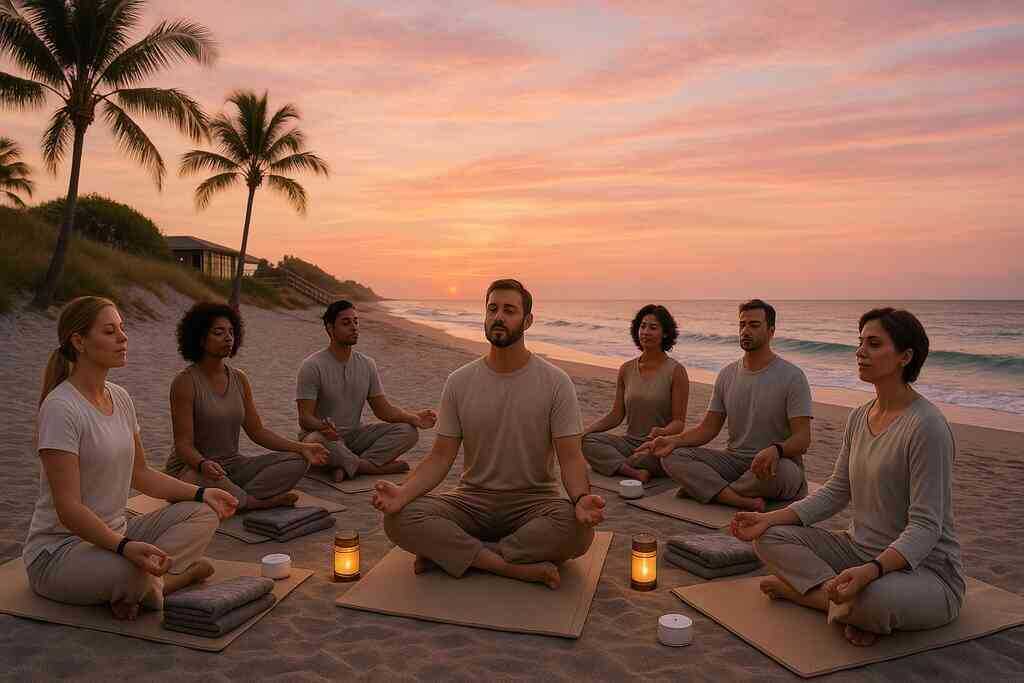
Nighttime meditation groups convene in softly lit studios where ocean tones play at low volume. Instructors lead guided meditation for better sleep, teaching patients to observe thoughts without judgment, then release them into imagined tides. Attention gently shifts toward body awareness, priming parasympathetic dominance and easing tense muscles. Next, progressive muscle relaxation for patients moves from toes to scalp, squeezing and releasing each region. The sequence sends clear safety signals, reducing cortisol that fuels insomnia.
Importantly, these practices complement psychotherapy rather than compete with it. Traumatic memories often surface after daytime processing; evening relaxation helps contain that emotional residue. Consistency breeds conditioned calm, so participants receive audio recordings for use at home, maintaining continuity outside sessions. Many report falling asleep halfway through rehearsed scripts within two weeks. Such rapid gains demonstrate how holistic sleep methods in Florida rehab centers can rival pharmacological solutions without side effects.
White noise therapy and supportive bedding environments
Environmental tweaks can transform restless nights into rejuvenating slumber, especially during early alcohol detox and sleep restoration. Staff evaluate each living space, ensuring mattresses cushion pressure points while maintaining spinal alignment. Blackout curtains block ambient glare, essential for a stable melatonin cascade. White noise machines hum at frequencies that mask hallway sounds, preventing micro-arousals that sabotage REM consolidation. Together, these elements craft supportive bedding environments in treatment centers where comfort equals compliance.
Furthermore, patients experiment with various soundscapes-from gentle rain to soft fan oscillations-to discover personal preferences. Data show that when noise remains consistent, the brain learns to ignore it, creating a buffer against sudden disturbances. Counselors also teach nightly rituals such as lowering room temperature slightly, promoting deeper slow-wave sleep. By blending science and comfort, the intervention reinforces that quality rest is not a luxury but essential medicine within recovery programs.
Mindfulness bedtime rituals crafted on Delray Beach
Sunset strolls along the shoreline anchor circadian rhythm reset during IOP by exposing eyes to gradually fading light. As waves rhythmically crash, clients practice mindfulness bedtime rituals at Delray Beach, syncing breaths with swells and grounding thoughts in sensory details. This natural progression from bright day to dim evening cues pineal melatonin release without supplements. Participants then write three gratitude statements, shifting cognitive focus from stress to positive reflection. These small acts collectively nurture nightly serenity.
Rainy evenings offer indoor alternatives that maintain ritual integrity. Scented candles with beach-inspired aromas evoke similar calm, while soft stretching loosens residual tension. The predictability of sequence signals the limbic system to deactivate fight-or-flight circuits. Over time, patients associate the ritual with safe sleep onset, reducing reliance on external sleep aids. Graduates often continue these practices, confirming their portability beyond the program.
Breathing exercises that calm nighttime cravings
Cravings frequently spike when silence amplifies residual dopamine imbalances, but tactical breathing can override that storm. Counselors teach four-part box breathing and extended exhale methods, both proven to activate vagal tone. As carbon dioxide levels adjust, heart rate slows, granting immediate relief from restless urgency. Clients rehearse these breathing exercises for nighttime calm during group simulations, then deploy them when urges arise in real bedrooms. The technique pairs physiological regulation with cognitive distraction, doubling effectiveness.
For additional support, individuals may choose to contact experts near Palm Beach for sleep coaching, ensuring personalized guidance remains only a phone call away. This direct line underscores our commitment to accessible care, especially during vulnerable late-night hours. When combined with earlier interventions, controlled respiration fortifies relapse prevention through healthy sleep rhythms. Patients awaken clearer, proving that rested bodies fuel resilient minds. Confidence grows, and the feedback loop of success continues without chemical assistance.
Lifestyle Anchors that Fortify Nighttime Recovery
Nutrition protocols that balance natural melatonin
Proper fueling patterns give the pineal gland raw materials for restful chemistry. Clinicians at our Delray Beach IOP teach clients to combine tryptophan-rich turkey, magnesium-dense pumpkin seeds, and complex carbohydrates at dinner. This blend supports balancing melatonin naturally in rehab, helping sleepers drift without synthetic aids. Counselors also spotlight hidden saboteurs such as late caffeine, spicy food, and sugary desserts that spike cortisol. Patients track meals in digital logs, then compare sleep graphs to identify nourishing victories.
Education continues with culinary demonstrations inside the wellness kitchen. Participants learn to season vegetables with calming herbs like chamomile and lemon balm instead of heavy sauces. Hydration plans emphasize mineral water over diuretics, stabilizing nighttime electrolytes. Because nutrition and sleep quality in recovery programs are inseparable, dietitians collaborate with therapists weekly. Small adjustments, repeated consistently, compound into brighter mornings and stronger therapy engagement.
Yoga nidra and gentle movement for evening wind down
Many individuals crave a physical ritual that signals the nervous system to power down. Yoga nidra sessions at intensive outpatient programs provide that bridge, guiding bodies from active tension to tranquil stillness. Instructors cue slow diaphragmatic breathing, then lead body-scan visualizations that mimic stages of non-REM sleep. Research shows twenty minutes of nidra can equal one full hour of light rest, a persuasive statistic for skeptical newcomers. Over time, clients report falling asleep faster and waking less often.
Gentle stretching follows nidra, releasing lactic acid accumulated during strength training or mindfulness walks. Movements stay low-impact to protect joints recovering from substance-induced inflammation. Therapists encourage participants to note which postures ease specific cravings, creating personalized evening flow charts. Such customization exemplifies our specialized addiction care with holistic rest strategies, elevating standard exercise recommendations into therapeutic precision. Graduates often continue the sequence at home, proving portability boosts adherence.
Screen time reduction and blue light management
Phones and tablets bombard retinas with wavelengths that suppress melatonin for hours. Therefore, IOP in Delray Beach implements screen time reduction for improved rest as a measurable treatment goal. Clients activate night-shift filters one hour before lights-out and store devices outside bedrooms. Staff offer laminated reading materials and low-lux lamps as healthier alternatives to scrolling feeds.
We also teach practical hacks for unavoidable late-evening work. Blue-blocking glasses, quick email batching, and scheduled social media windows minimize circadian disruption. Participants analyze wearable data to witness how fifteen screen-free minutes can lengthen deep sleep by measurable percentages. These insights transform abstract science into personal motivation. Consistent compliance soon becomes second nature, reinforcing boundary skills useful beyond discharge.
Group workshops on healthy sleep habits
Peer synergy accelerates behavior change, so intensive outpatient programs in Delray Beach host weekly group workshops on healthy sleep habits. Facilitators blend evidence summaries with interactive challenges, such as designing the ideal bedroom on poster boards. Friendly competitions reward the quietest decibel readings or the most creative wind-down playlists. The social dynamic turns habit formation into communal fun rather than lonely discipline.
During breakout circles, participants troubleshoot shared barriers like noisy roommates or irregular work shifts. Veterans of earlier cohorts return as mentors, showing newcomers their tracked progress since graduation. This loop fosters accountability and celebrates progress openly. Workshops also introduce community resources, guiding attendees toward specialized addiction care with holistic rest strategies. By the final week, every client presents a personalized sleep charter, solidifying ownership of nightly wellness.
Chronic pain and sleep management within IOP care
Pain often lingers after detox, turning mattresses into battlegrounds instead of sanctuaries. Our rehabilitation centers integrate chronic pain and sleep management in IOP through multidisciplinary teamwork. Physical therapists teach joint-friendly positions using supportive pillows, while psychologists apply cognitive reframing to reduce catastrophizing thoughts. Non-opioid medications are timed to avoid REM suppression, demonstrating precise pharmacological stewardship.
Biofeedback sessions show clients real-time muscle tension during bedtime rehearsals. As they watch graphs drop, confidence rises. Meanwhile, mindfulness bedtime rituals at Delray Beach merge with heat therapy packs, soothing both nerves and anxiety. The synergy helps patients reclaim agency over bodies once numbed by substances. Rested muscles heal faster, creating a virtuous cycle that supports long-term recovery momentum.

Rested Today Resilient Tomorrow
Relapse prevention through healthy sleep rhythms
Consistent sleep functions as an invisible guardian that guards sobriety with quiet strength. Each full sleep cycle refuels executive control, allowing calmer responses when triggers emerge. Scientists report that rested brains regulate dopamine more smoothly, cutting impulsive cravings before they escalate. Therefore, delray beach IOP clinicians place sleep tracking alongside cravings logs, because both metrics predict relapse risk. When patients notice fewer nighttime awakenings, motivation to protect routines intensifies.
Therapists weave relapse prevention through healthy sleep narratives into every group, highlighting how even minor bedtime deviations sabotage progress. Clients rehearse relaxation drills until they activate automatically during restless moments. This procedural memory, forged in deep sleep, becomes a behavioral shield long after discharge. By treating sleep rhythms as non-negotiable, intensive outpatient programs in Delray Beach create a proactive defense rather than a reactive scramble. Graduates often describe this habit as a lifelong anchor that keeps recovery steady through unpredictable storms.
Post discharge resources and IOP near you with sleep support
Leaving structured care can unsettle even the most prepared mind; however, robust community tools quickly restore balance. Counselors introduce alumni to many supports, including curated articles outlining top mental wellness tactics for nightly resilience. The resource list reminds readers that evidence-based sleep strategies remain accessible, whether they live locally or relocate. Interactive webinars break complex science into practical routines, making continued learning both engaging and convenient. Participants share victories, creating momentum that reinforces bedtime discipline.
Delray Beach Intensive Outpatient Programs also coordinate referrals to partner wellness centers that offer evening check-ins. These flexible touchpoints replicate IOP accountability while respecting new schedules. For individuals in remote regions, therapists identify reputable intensive outpatient programs near you with sleep support, ensuring continuity of specialized guidance. Alumni groups meet virtually, providing peer companionship during vulnerable late-night hours. Such support layers build confidence, so setbacks become growth opportunities instead of relapse triggers.
A future where mental health and sleep thrive together
Public awareness increasingly recognizes that mental health facilities must value sleep as essential medicine, not a luxury. Research partnerships now explore personalized chronotherapy, predicting optimal light exposure for each genetic profile. As findings mature, rehabilitation centers will translate data into everyday tools, eliminating guesswork from nightly routines. Delray Beach leaders already pilot wearable integrations that adjust room lighting automatically when circadian drift appears. This forward momentum promises humane, adaptive treatment landscapes.
Ultimately, society will measure wellness by the alignment of daylight actions and nighttime restoration. Families will discuss circadian health as naturally as nutrition or exercise. Employers will respect recovery-friendly schedules, reducing after-hours demands that erode stability. When that culture arrives, fewer people will need crisis care because protective habits will start early. Until then, Delray Beach Intensive Outpatient Programs stand ready to guide every patient toward restful nights and resilient tomorrows.
Frequently Asked Questions
Question: How does Delray Beach IOP integrate personalized sleep assessments into its intensive outpatient programs?
Answer: Every new client begins with a comprehensive, science-driven sleep assessment that maps chronotype, bedtime routines, nightmare frequency, caffeine intake, and wearable data. Our clinicians then align therapy blocks, meal times, and medication dosing with your natural energy peaks-an approach called personalized sleep assessments at wellness centers. By synchronizing daily programming with your circadian rhythm, we boost engagement, sharpen focus, and accelerate healing. Over the course of treatment, we refine these plans using weekly check-ins and objective sleep metrics, proving why Delray Beach IOP sleep therapy consistently outperforms one-size-fits-all models.
Question: What restorative rest strategies for recovery can I expect during alcohol detox and sleep restoration at your Florida rehab center?
Answer: Alcohol detox often triggers REM rebound, vivid dreams, and fragmented rest. Our Florida rehab centers counter these challenges with a multilayered protocol: non-habit-forming supplements, evening protein snacks, timed magnesium, breathing exercises for nighttime calm, and guided meditation for better sleep. We also collaborate with nearby detox facilities to ensure medications never sabotage your bedtime. By blending behavioral sleep interventions in rehab with compassionate medical oversight, we transform restless nights into a powerful shield against cravings and relapse.
Question: In the blog Sleep Methods at Delray Beach Intensive Outpatient Programs, you discuss circadian rhythm reset during IOP-how is this achieved day to day?
Answer: Our circadian rhythm reset during IOP relies on strategic light exposure, consistent lights-out, and chronotype-sensitive scheduling. Sunrise walks along Delray Beach jump-start serotonin production, while dusk mindfulness bedtime rituals cue melatonin naturally. Early birds process groups before noon; night owls tackle analytic work later. Wearable tech tracks sleep stages so you can see measurable gains. This daily rhythm rebuilds neurochemical balance, proves the mental health and sleep connection in IOP, and makes therapy feel energizing instead of exhausting.
Question: Do you offer trauma-informed sleep coaching and CBT-I for substance recovery within your Delray Beach intensive outpatient program?
Answer: Absolutely. Dual-diagnosis clients receive trauma-informed sleep coaching that blends grounding techniques, weighted blankets, and secure bedroom layouts with evidence-based EMDR. Simultaneously, licensed therapists deliver CBT-I for substance recovery, dismantling unhelpful beliefs like “I will never rest sober” and teaching stimulus control, sleep restriction, and cognitive restructuring. This combination calms hyper-arousal, reduces nighttime flashbacks, and rewires insomnia at its root-one reason intensive outpatient programs in Delray Beach are considered leaders in compassionate sleep counseling in rehabilitation.
Question: How do supportive bedding environments and white noise therapy at your treatment center improve relapse prevention through healthy sleep?
Answer: Our treatment centers feature premium mattresses, blackout curtains, optimal room temperatures, and customizable white noise therapy near Delray Beach. These supportive bedding environments eliminate micro-arousals that fragment REM sleep, allowing the brain to consolidate coping skills learned during the day. Because rested minds regulate dopamine more smoothly, cravings shrink and decision-making strengthens-core elements of relapse prevention through healthy sleep. Clients often report their first full night of uninterrupted rest in years, reinforcing the belief that recovery can feel comfortable as well as empowering.
