Awakening the Emotional Tides
Why Mood Shifts Define the First Steps of Recovery
Mood shifts during outpatient recovery often feel like unpredictable waves, yet they mark essential neurological healing. Early sobriety disrupts brain chemistry, so emotions can swing from euphoria to despair within hours. Clients sometimes fear these fluctuations, believing they signal failure, but they actually reveal renewed sensitivity. Identifying and labeling each feeling becomes the first exercise in emotional regulation at Delray Beach IOP. Through guided reflection, individuals learn that coping with mood swings in rehab involves curiosity, not judgment, which lowers relapse risk.
Intensive outpatient depression care teaches that mood volatility roots itself in stress hormones like cortisol. When substances leave the bloodstream, cortisol initially spikes, magnifying irritability and anxiety. Group psychoeducation clarifies this biological process so clients stop blaming character flaws. Recognizing that the limbic system is recalibrating provides hope and patience. Armed with this insight, participants embrace every emotional surge as proof of progress toward healthier neurochemistry.
Delray Beach IOP as a Safe Harbor for Emotional Regulation
Tucked between tropical palms and soothing ocean breezes, the center offers a sensory buffer that naturally calms the nervous system. Clinicians integrate dialectical behavior therapy, teaching clients to ride emotional waves with distress-tolerance skills. A daily schedule balances psychoeducational groups, expressive arts, and mindful beach walks, which ground participants in present-moment awareness. These activities lower sympathetic arousal, allowing the prefrontal cortex to regain executive control. As a result, fragile moods settle, and clients experience stability they once thought impossible.
Therapists underscore secure attachment by maintaining consistent eye contact, validating feelings, and reinforcing safety. This relational approach counters the isolation that fuels substance misuse. Every staff member, from medical director to yoga instructor, follows trauma-informed protocols. Their unified mission cements Delray Beach IOP as a trustworthy refuge. Clients repeatedly describe the environment as the first place where their emotions feel both welcomed and contained, a cornerstone for sustained recovery.
For newcomers exploring options, the Delray Beach IOP overview highlights these evidence-based strategies in detail. Prospective clients discover how individualized care plans weave together pharmacotherapy, CBT, and holistic modalities. Transparent program descriptions reduce uncertainty, which itself stabilizes mood. Reading success stories online offers social proof that change is attainable. Hope blooms when people realize a supportive harbor truly exists.
Setting Expectations for Intensive Outpatient Programs in Delray Beach
Understanding program structure lowers anxiety, a critical factor in emotional regulation. Sessions typically run several hours, multiple days weekly, allowing participants to practice new skills between meetings. Clinicians assign mood-tracking journals, encouraging real-time awareness and pattern recognition. Evening family workshops teach loved ones how to respond to sudden irritability, preventing conflict escalation. Clear expectations create psychological safety, enabling deeper therapeutic work.
Core curriculum covers relapse prevention, mindfulness practices in IOP, and dual-diagnosis mood disorder education. Clients learn specific breathing techniques that deactivate the amygdala within minutes. Nutritionists explain how balanced macronutrients support serotonin production, complementing psychopharmacology when prescribed. Peer groups share lived experiences about managing triggers at local social gatherings. With every lesson, confidence grows, and emotional storms shorten.
Anyone seeking more program specifics can explore intensive outpatient programs in Delray Beach for a thorough breakdown of schedules and modalities. The resource outlines admission steps, insurance options, and aftercare planning. Clear information empowers informed consent, which enhances therapeutic alliance. By demystifying the process, Delray Beach IOP nurtures calm anticipation rather than fearful guessing. Expectations align with reality, reducing stress and safeguarding early recovery.

Navigating the Swells of Change
Biopsychosocial Roots of Mood Volatility in Dual-Diagnosis Care
Early mood shifts during outpatient recovery confuse many clients, yet biology, psychology, and environment all contribute. Substance withdrawal lowers dopamine while spiking cortisol, so agitation rises quickly. Concurrent depression or anxiety amplifies this chemical chaos, producing dual diagnosis mood disorders that feel unmanageable. Intensive outpatient programs in Delray Beach teach that these reactions are expected, not personal failings. Recognizing the biopsychosocial puzzle reduces shame and encourages stable engagement.
Florida IOP mental health support also explores social stressors such as financial worries and family conflict. Therapists map each trigger alongside corresponding neurotransmitter changes, creating an integrated treatment blueprint. This approach highlights why mood shifts during outpatient recovery require multifaceted solutions. Clients learn to match internal sensations with external pressures, building emotional literacy. For deeper education, clinicians often reference mental health care at Delray Beach IOP, ensuring every participant accesses specialized expertise.
Cognitive-Behavioral Charts and Mindfulness Compasses for Sobriety
Cognitive behavioral tools for sobriety act like nautical charts, guiding clients through distorted thinking that worsens mood swings. Participants document automatic thoughts, label cognitive distortions, and then replace them with balanced statements. This repetitive practice strengthens neural pathways that encourage calm decision-making. Over time, emotional regulation at Delray Beach IOP becomes instinctive rather than forced. Structured worksheets turn abstract theory into tangible daily actions.
Mindfulness practices in IOP complement cognitive restructuring by anchoring attention to breath, body, and immediate surroundings. Short meditations calm the amygdala, lowering reactivity toward cravings. Clients track sensations without judgment, which improves coping with mood swings in rehab. For additional exercises, counselors share anxiety management tools on Delray Beach IOP blog during group sessions. The blend of CBT and mindfulness forms a powerful compass that keeps recovery on course.
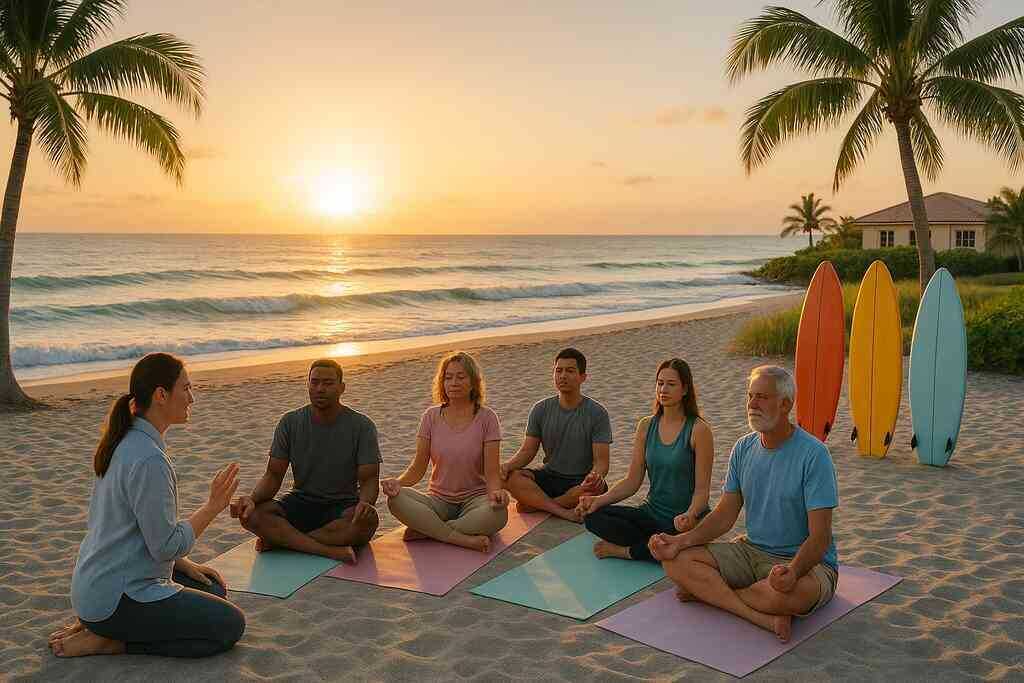
Surf Therapy and Ocean-Side Mindfulness Unique to Rehab in Delray Beach
Rehab in Delray Beach leverages its shoreline to provide surf therapy for emotional health, an experiential modality backed by emerging evidence. Riding waves demands present-moment focus, integrating physical exertion with rhythmic breathing. Clients report that saltwater immersion washes away intrusive thoughts, turning panic into exhilaration. The ocean’s predictable ebb and flow mirrors emotional tides, fostering acceptance. Staff instructors ensure safety and tailor drills to each fitness level.
Between lessons, participants practice walking meditations along the sand, absorbing negative ions that naturally boost serotonin. These holistic therapies for mood stability rely on sensory engagement rather than talk alone, appealing to clients who feel therapy fatigue. Many describe ocean-side mindfulness as the first place they truly inhale hope. Such embodied learning transforms abstract skills into lived experience, embedding calm in muscle memory.
Nutrition, Sleep Hygiene, and Circadian Alignment for Mood Stability
Balanced meals rich in omega-3 fats, B-vitamins, and complex carbohydrates fuel neurotransmitter synthesis. Nutrition and mood recovery programs therefore include culinary classes where clients prepare anti-inflammatory dishes. Dietitians explain how blood-sugar crashes mimic depressive episodes, urging regular eating schedules. Hydration protocols also prevent fatigue that masquerades as despair. Food becomes medicine, not mere fuel, reinforcing sobriety goals.
Even the best diet falters without restorative sleep, so clinicians teach sleep hygiene in addiction treatment as a core relapse prevention tool. Blue-light limits, consistent bedtimes, and pre-sleep stretching routines realign circadian rhythms disrupted by substances. Clients practice gratitude journaling to quiet racing thoughts at night. For detailed guidance, mentors provide sleep hygiene strategies during IOP as a take-home reference. Combined with morning light exposure, these strategies stabilize hormones and smooth emotional peaks.
Pharmacotherapy and Trauma-Informed Support in a Florida IOP Setting
Some individuals require pharmacotherapy in outpatient setting to correct severe chemical imbalances. Psychiatrists prescribe evidence-based mood stabilization medications, monitoring plasma levels closely. Clients receive education about side effects, ensuring informed consent and adherence. Medication, however, is framed as a bridge, not a crutch, reinforcing active skill building. Regular reviews track progress and adjust dosages as necessary.
Trauma informed outpatient services ensure medications are delivered within a compassionate framework. Clinicians avoid triggering language and respect bodily autonomy during assessments. Personalized mood disorder treatment plans include somatic grounding, art therapy, and EMDR. This integrative stance recognizes that unresolved trauma often drives substance use. As trust grows, pharmacology and psychotherapy synergize, producing durable emotional balance.
Group, Family, and Peer Currents Steering Emotional Balance
Group therapy emotional balance emerges when peers witness each other’s raw feelings without judgment. Shared stories normalize fear, guilt, and sudden tears, replacing isolation with solidarity. Facilitators teach active listening, ensuring every voice matters. When conflicts surface, members practice assertive communication rather than impulsive reactions. Such rehearsals translate smoothly into outside relationships.
Family counseling for mood changes further strengthens resilience by rebuilding fractured bonds. Loved ones learn to validate feelings instead of offering quick fixes that spark frustration. Sessions address codependency patterns and set healthy boundaries. Peer support for emotional resilience continues post-treatment through alumni meetings and online forums. This social scaffold sustains recovery when professional contact decreases.
Real-Time Mood Tracking and Relapse Prevention Technology
Clinicians introduce digital journals that ping users three times daily, asking for quick mood ratings. Relapse prevention mood tracking highlights subtle shifts before crises erupt. Data populates colorful graphs visible to both client and therapist, promoting transparency. When negative trends appear, intervention plans activate immediately. Accountability feels empowering rather than punitive.
Artificial intelligence within the app suggests breathing exercises, inspirational videos, or music playlists tailored to current emotions. Aftercare mood management plans sync seamlessly with these prompts, offering consistency during transition phases. Clients celebrate improved scores as personal victories, reinforcing sustained engagement. Technology thus transforms recovery from abstract goal to interactive game, where progress becomes visible and motivating.
Seasonal Stressors and Environmental Triggers Near the Coast
Living near water offers tranquility, yet coastal storms or tourist surges can still unsettle sensitive nervous systems. Seasonal stressors like humidity changes affect sleep quality, influencing daytime mood. Clinicians teach weather-based contingency planning, urging indoor exercise on stormy days. Light boxes counter overcast gloom, maintaining serotonin balance. Preparedness prevents minor irritations from snowballing into relapse risk.
Environmental cues such as bar patios or beach festivals may revive memories of past drinking sprees. Clients rehearse exit strategies and assertive refusals before venturing out. Staff distribute checklists for identifying sensory triggers like rum aromas or loud music. For extra guidance, graduates review identifying triggers near the beach to refresh coping strategies. In this way, coastal living becomes a source of joy, not jeopardy.
Anchoring Calm Horizons
Personalized Aftercare Mood Management Plans
Individualized aftercare plans act like nautical charts for the months that follow intensive outpatient programs in Delray Beach. Clinicians collaborate with each participant to map daily routines, anticipated stress points, and preferred coping styles. Together they refine relapse prevention mood tracking apps, ensuring push notifications arrive at realistic intervals. Each plan lists backup therapists and crisis lines, reducing decision fatigue during emotional spikes. By weaving accountability with autonomy, the blueprint promotes steady confidence.
The document also schedules quarterly check-ins that reassess medication efficacy, sleep hygiene practices, and nutrition adjustments. Clients bring recent mood data, transforming subjective feelings into actionable patterns. When indicators show rising anxiety, the team suggests immediate interventions such as extra breathwork sessions or brief return visits. This proactive stance prevents small dips from snowballing into destabilizing episodes. Consequently, responsive aftercare mood management plans safeguard progress amid life’s unpredictability.
Alumni and Peer Networks for Lifelong Emotional Resilience
Graduates soon realize that peer support for emotional resilience delivers something professional sessions cannot: relatable stories spoken in the same recovery dialect. Weekly alumni circles offer space to vent about job searches, relationship tensions, or sudden nostalgia for former habits. Hearing diverse solutions sparks fresh ideas and dissolves isolation. Moreover, the shared laughter that follows a sobering confession strengthens neural pathways linked to joy.
Delray Beach IOP also hosts seasonal beach clean-ups, turning service work into a team-building exercise. Physical activity under open skies releases endorphins while reinforcing sober camaraderie. Participants often exchange numbers, forming micro-groups that text daily affirmations. If someone flags low motivation on the group chat, others respond with ride offers to meetings or quick mindfulness audios. This grassroots safety net proves invaluable when formal therapy hours diminish.
Self-Compassion Training and Life-Skills Integration
Early recovery voices often echo with self-criticism, so counselors introduce self compassion training in rehab to soften that tone. Guided meditations encourage clients to treat inner dialogue like they would a tender friend. Over time, kinder self-talk lowers cortisol spikes and widens the window of emotional tolerance. Clients then practice writing forgiveness letters to themselves, a ritual that many describe as transformative.
Practical life skills for emotional wellness accompany this internal shift. Budgeting classes alleviate financial panic, while conflict-resolution workshops rehearse assertive language. Culinary demonstrations teach quick, mood-supportive meals that fit hectic schedules. Each lesson concludes with a reflection circle, linking newfound competence to decreased mood volatility. Thus, holistic mastery replaces frantic improvisation with strategic self-care.
Connecting to Community Mental Health Facilities and Wellness Centers
Sustainable growth depends on resources beyond any single facility, so staff curate referrals to vetted mental health facilities and local wellness centers. Counselors introduce directories that help graduates locate yoga studios, meditation groups, and volunteer opportunities within walking distance. They also review insurance details, ensuring seamless continuity of therapeutic services. These practical steps eliminate bureaucratic friction that could discourage follow-through.
During the final week, clinicians arrange warm handoffs, sometimes inviting new providers to attend a session. This face-to-face introduction reduces social anxiety and accelerates rapport. Clients leave with confirmed appointments, transportation plans, and a printed list of backup contacts. Knowing multiple safety nets exist bolsters confidence, further decreasing relapse risk. As a result, community integration feels exciting rather than overwhelming.
Measuring Progress and Celebrating Milestones Beyond Intensive Outpatient Programs
Tracking growth maintains motivation, so graduates select personalized metrics like consecutive mindfulness minutes or balanced-budget months. Digital dashboards convert these numbers into colorful graphs that celebrate upward trends. When milestones emerge-perhaps three hundred mood logs completed-the community rejoices with symbolic tokens such as hand-painted shells. These tangible rewards anchor abstract achievements in physical memory.
Celebrations also serve diagnostic purposes. If progress plateaus, mentors review data to identify hidden stressors or neglected self-care rituals. Immediate course corrections keep emotional regulation at Delray Beach IOP momentum alive long after discharge. Anyone seeking guidance at any point can easily contact Delray Beach outpatient team for refreshed strategies or simply a reassuring conversation. In this way, milestones mark not endings but vibrant checkpoints along a lifelong voyage toward balanced living.
 Frequently Asked Questions
Frequently Asked Questions
Question: How does Delray Beach IOP help me cope with mood shifts during outpatient recovery?
Answer: Mood shifts during outpatient recovery are normal because your brain and body are recalibrating after substance use. At Delray Beach Intensive Outpatient Programs, we combine Florida IOP mental health support with evidence-based therapies like dialectical behavior therapy (DBT) and cognitive behavioral tools for sobriety. Clinicians first explain the biology behind cortisol spikes so you stop blaming character flaws. Then we practice distress-tolerance skills, guided beach meditations, and personalized mood tracking that alerts your care team to sudden changes. This layered approach transforms coping with mood swings in rehab from a guessing game into a predictable, skill-driven process you can trust.
Question: What emotional regulation techniques will I actually learn in the intensive outpatient programs in Delray Beach?
Answer: Emotional regulation at Delray Beach IOP is taught through a structured curriculum that blends mindfulness practices in IOP with practical life skills. You will master paced-breathing drills that deactivate the amygdala in under three minutes, CBT thought-logs that turn distorted beliefs into balanced self-talk, and nutrition and mood recovery programs that stabilize blood sugar and serotonin. Sleep hygiene in addiction treatment is also covered, along with self compassion training in rehab to soften harsh inner dialogue. By weaving these techniques into daily routines, our IOP in Delray Beach equips you to handle triggers at work, home, or the beach with confidence.
Question: In the blog post Mood Shifts at Delray Beach Intensive Outpatient Programs, surf therapy sounded intriguing. How does surf therapy for emotional health fit into my treatment plan?
Answer: Surf therapy for emotional health is one of our signature holistic therapies for mood stability. Under the supervision of certified instructors, you learn to match your breath with the rhythm of incoming waves, which naturally mirrors mindfulness exercises. Physical exertion releases endorphins, while the ocean’s predictable ebb and flow reinforces acceptance of emotional tides. Sessions are scheduled alongside group therapy emotional balance workshops, so insights gained on the board are processed immediately on land. This mind-body integration accelerates recovery and makes rehab in Delray Beach a uniquely uplifting experience.
Question: Can family counseling for mood changes really improve outcomes for dual diagnosis mood disorders?
Answer: Absolutely. Dual diagnosis mood disorders thrive on isolation and misunderstanding. Our family counseling for mood changes educates loved ones on the biochemical roots of anxiety and depression, removing blame from the conversation. Together you’ll practice assertive communication, boundary setting, and relapse-prevention planning. When the home environment supports emotional regulation, stress hormones decline, medication adherence improves, and overall treatment engagement rises. Families leave with concrete action plans that extend the safety of our rehabilitation centers into your living room.
Question: What aftercare mood management plans and relapse prevention mood tracking tools do you provide once I complete the program?
Answer: Graduates receive personalized aftercare mood management plans that include digital journals pinging you for quick check-ins three times a day. These relapse prevention mood tracking apps sync with your therapist’s dashboard so small dips trigger immediate outreach. You’ll also schedule quarterly medication reviews, nutrition tune-ups, and optional booster sessions at our wellness centers. Peer support for emotional resilience continues through weekly alumni circles and seasonal beach clean-ups. All these services ensure that even after you leave our treatment centers, the Delray Beach IOP network keeps you anchored to calm horizons.
