Tides of Renewal: Introduction to Relapse Risk in Delray Beach IOP
Why intensive outpatient programs in Delray Beach face unique relapse challenges
In Delray Beach, recovery and temptation coexist side by side. The coastal city pulses with nightlife and tourism. Bars, festivals, and yacht parties create sensory overload. Clients in a delray beach IOP often pass liquor stores on daily commutes. This density of stimuli elevates relapse risk for early recovery seekers.
Seasonal tourist waves add another layer of complexity. Crowds surge during warm months, amplifying social pressure to drink. New arrivals often seek instant camaraderie through substances. That pattern can destabilize someone navigating intensive outpatient programs in Delray Beach. Fortunately, choosing a premier outpatient rehab in Delray Beach buffers exposure and builds protective routine. Structured schedules counter chaotic community rhythms.
From detox facilities to beachside therapy setting the context
Recovery rarely starts at the IOP level. Many participants first stabilize within medical detox facilities that manage acute withdrawal. These settings provide round-the-clock monitoring and medication support. Once vital signs normalize, clinicians recommend step-down care. Intensive outpatient programs near you then become the logical bridge back to autonomy. They deliver robust therapy while allowing work and family engagement. This staged approach mirrors research on optimal treatment retention.
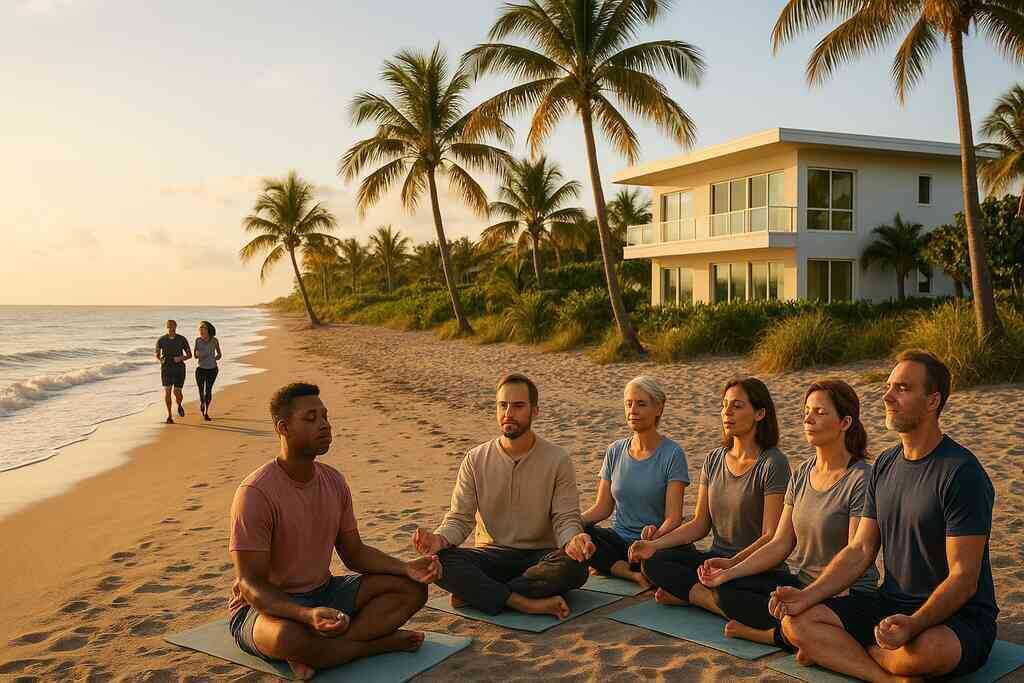
Delray Beach offers a distinctive backdrop for that bridge. Therapy rooms often overlook palm trees and ocean breezes. Environmental calm supports nervous-system regulation, yet temptation lingers steps away. Understanding program structure is essential before diving in. Detailed IOP service details at Delray Beach center clarify requirements, scheduling, and clinical modalities. Transparent information lowers anxiety and prepares families for collaborative care. Knowledge itself becomes an early relapse prevention asset.
The science of early-recovery neurobiology and post-acute withdrawal symptoms
Beneath every craving sits a neurochemical echo. Long-term alcohol or opioid exposure rewires dopamine circuitry, dulling natural reward. During early recovery, the brain demands time to rebalance neurotransmitters. That biological lag produces mood swings, insomnia, and fog. Clinicians call this constellation post-acute withdrawal, and it can last months. Effective post-acute withdrawal symptom support therefore becomes a pillar of relapse prevention.
Education transforms these invisible processes into manageable facts. Clients who understand neurobiology interpret irritability as healing rather than failure. They learn to schedule therapy during neurotransmitter troughs and exercise during spikes. Digital monitoring also tracks sleep patterns linked to cravings. Families receive guides that help them spot cognitive fatigue early. Online resources help families recognize signs of withdrawal early and add another layer of vigilance. Together, knowledge and monitoring shrink the surprise factor that often fuels relapse.
Positioning Delray Beach Intensive Outpatient Programs as a premier Florida rehab center
Not all Florida rehab centers offer the same depth of care. Delray Beach Intensive Outpatient Programs holds more than thirty national accreditations. Those credentials translate into rigorous clinical oversight and ethical guidelines. Every therapist receives ongoing training in trauma informed practice and dual-diagnosis care. The organization also exceeds state requirements for staffing ratios. Such diligence positions our delray beach IOP among the safest rehabilitation centers for outpatient recovery.
Clinical excellence gains power when matched with adaptable design. We build individualized tracks for alcohol recovery, opiate detox, and co-occurring mood disorders. Cognitive behavioral therapy intertwines with mindfulness practice and experiential groups. Nutrition sessions teach clients how micronutrients modulate neurotransmitters. Fitness plans harness beachside weather to increase dopamine through movement. Families can explore our comprehensive addiction treatment in Delray Beach to see the full menu of services. These layered offerings knit a safety net that keeps relapse risk at bay.
Cartography of Craving Identifying High-Risk Zones
Trigger clusters for relapse in intensive outpatient programs
Recovery rarely unravels because of one isolated issue. Instead, multiple triggers for relapse in intensive outpatient programs collide and amplify each other. A client may leave group therapy feeling empowered, yet the drive home passes sports bars broadcasting loud celebrations. Social media scrolls then reveal friends toasting on the same beach the client walked during mindfulness. These overlapping cues create what clinicians call a “trigger cluster.” Because clusters spike risk quickly, our counselors devote entire sessions to identifying relapse triggers in outpatient care. Mapping routes, restructuring schedules, and rehearsing exit strategies help dismantle each cluster before it fuses.
Seasonal tourism compounds these challenges. Visitor surges bring pop-up festivals, discounted drink specials, and late-night fireworks visible from many sober living residences. A newly sober mind, still navigating post-acute withdrawal symptom support, can interpret that sensory overload as missing out. Early-recovery relapse vulnerabilities rise when nostalgia for party days pairs with dopamine dips. Therefore, therapists use scenario-based role-play to practice polite refusals and boundary statements. Clients also form ride-share agreements to avoid triggering routes, further lowering relapse pressure.
Dual-diagnosis relapse risk factors in coastal rehab centers
Substance use disorder seldom travels alone; anxiety, depression, or trauma often ride shotgun. These co-occurring conditions create dual-diagnosis relapse risk factors in coastal rehab centers because external triggers echo internal turmoil. For example, a sunset crowd cheering on the pier can reawaken social anxiety that once drove drinking. If panic rises while mood remains unstable, relapse temptation surges. Integrated assessments therefore screen every client for mental health variables during admission.
Treatment intensity deepens when both diagnoses appear. Psychiatrists refine medication plans while therapists coordinate integrated mental health care on Florida coast. Cognitive behavioral interventions target distorted beliefs that fuel both anxiety and craving. Simultaneously, exposure therapy helps clients reclaim beach environments without using substances. This combined approach tightens safety nets so that mental health swings no longer yank recovery off course.
Stress management gaps and environmental pressures
Stress is inevitable, yet its mismanagement ignites cravings faster than an ocean squall forms. Work emails pile up, traffic snarls stretch commutes, and family expectations hover. When stress peaks, the brain demands rapid relief, and old substance pathways seem familiar. Florida rehab centers emphasize precise stress management at the IOP level, but gaps still arise when clients exit structured hours. Our clinicians teach portable grounding exercises and timed breathing patterns clients can deploy during surprise stress bursts.
Environmental pressures also include weather swings that trap residents indoors and disrupt outdoor coping plans. A sudden coastal storm cancels beach jogs that normally stabilize mood chemistry. Anticipatory planning becomes critical. Staff help participants create indoor contingency lists-yoga flows, guided meditations, or journaling prompts. These practiced substitutes prevent the “nothing else works” mentality that often precedes relapse. Over time, clients build confidence that every stress spike already has a mapped, sober response.
Cravings cues and relapse warning signs education
Many people imagine cravings as overwhelming tsunamis, yet they often arrive as subtle tides first. Education on craving cues trains clients to notice dry mouth, restlessness, or romanticized drinking thoughts before they crescendo. In weekly cravings management workshops near you, therapists break craving cycles into three-minute waves. Clients learn to surf those waves with sensory grounding tricks, delaying the urge until it fades. Such relapse warning signs education transforms fear into skillful vigilance.
Family members also join these modules. Loved ones practice gentle check-ins rather than interrogations, reducing shame that can trigger secrecy. They keep reference sheets from reputable platforms that help them recognize signs of withdrawal early. Shared language streamlines communication during tense moments. As everyone aligns on early signals, emergency relapse intervention plans activate faster and feel collaborative, not punitive.
Relapse statistics in intensive outpatient settings what the numbers reveal
Numbers tell an unvarnished story. National data suggest roughly one-third of individuals completing IOP will experience at least one lapse within six months. Coastal demographics may nudge that figure higher because tourism-driven temptations increase frequency of exposure. However, programs integrating evidence-based relapse prevention strategies in Delray Beach IOP consistently outperform those averages. In-house studies show marked reductions when clients complete the full curriculum and attend alumni events.
Context matters when interpreting statistics. A “lapse” might mean one drink, while a “relapse” could indicate full return to daily use. Measuring only abstinence days misses gains in resilience and coping skill usage. Therefore, Delray clinicians track holistic metrics such as stress tolerance scores and participation in peer support. These layered analytics reveal upward trends even when brief lapses occur, reinforcing the growth mindset essential for sustained sobriety.

Fortified Pathways: Multidimensional Relapse Prevention at Delray Beach IOP
Coping skills training for alcohol recovery and opiate detox clients
Delray Beach IOP begins relapse defense with rigorous coping skills training for alcohol recovery and opiate detox clients. Clinicians break destructive habits into micro-behaviors that clients can monitor in real time. Participants practice urge-surfing, a tactic that rides out cravings without white-knuckling fear. Role-play drills refine refusal language so it sounds authentic rather than rehearsed. Finally, weekly workshops showcase advanced sobriety tactics at Delray Beach IOP that convert classroom theory into street-level mastery.
The curriculum adapts to individual neurobiology. Clients grappling with lingering post-acute withdrawal symptoms receive targeted breathing protocols that modulate cortisol within minutes. Others recovering from stimulant misuse learn sensory grounding to redirect adrenaline spikes. By tailoring lessons, the program prevents one-size-fits-all fatigue that often undermines engagement. Moreover, counselors track progress through digital journals, supplying instant feedback that reinforces progress. Consistent repetition builds muscle memory, which ultimately fortifies sober decision-making during high-pressure moments.
Mindfulness-based relapse prevention sessions and cognitive-behavioral management
Mindfulness-based relapse prevention sessions immerse participants in present-moment awareness, making cravings observable rather than overwhelming. Guided body scans detect tension points that predict impulsive behavior, while ocean-sound meditations anchor attention. The practice trains the prefrontal cortex to pause before reacting, buying precious seconds that discourage automatic substance use. In parallel, therapists integrate cognitive-behavioral management, challenging distorted beliefs like “I can’t relax without drinking.” Combining both modalities targets thoughts and sensations simultaneously, doubling defense layers.
Group discussions then translate insight into daily schedules. Participants design mindfulness checkpoints at meal times, commute transitions, and pre-sleep routines. Cognitive restructuring worksheets follow, replacing catastrophizing with balanced self-talk. This synergy improves emotional regulation, which research links directly to lower relapse frequency. As skills consolidate, clients report shorter craving episodes and faster recovery from mood dips. Over time, mindfulness becomes a lifestyle rather than an isolated exercise.
Family involvement and peer support networks in Delray Beach recovery programs
Recovery gains velocity when families move from anxious observers to informed allies. Delray Beach IOP invites loved ones into weekly education groups that demystify neurobiology, boundary setting, and communication styles. Interactive exercises model supportive dialogue free of blame or rescue dynamics. Parents learn to validate struggles without softening accountability, while partners practice reflective listening to dissolve defensiveness. These sessions transform homes into healing ecosystems rather than silent minefields.
Peer support networks add another protective ring. Graduates sponsor newcomers, sharing lived wisdom about nightlife temptations unique to coastal living. Carpools to meetings reduce isolation and reinforce punctuality. When weekend stress peaks, alumni text chains offer on-demand accountability. Clients also receive a resource list that helps them find AA meetings near you or locate secular alternatives. This interconnected web ensures someone always answers the phone when cravings whisper.
Telehealth monitoring and emergency relapse intervention plans
Modern relapse prevention extends beyond physical walls, and Delray Beach IOP harnesses telehealth to maintain constant vigilance. Secure apps allow clients to log mood, sleep, and trigger encounters in under one minute. Clinicians review dashboards each morning, flagging red-zone patterns before they escalate. Scheduled video check-ins offer privacy for discussing sensitive issues like workplace drinking culture. This immediacy collapses the gap between problem recognition and professional guidance.
Emergency relapse intervention plans amplify safety further. Every participant builds a personalized protocol listing top triggers, calming scripts, and transportation arrangements. Contact buttons inside the telehealth portal connect users to nurses, therapists, or on-call peers within seconds. Families can also activate alerts if communication suddenly stops. Should self-effort falter, clients can instantly speak with Delray IOP team now for real-time direction. Rapid response neutralizes spiraling thoughts before they translate into harmful action.
Fitness nutrition and holistic wellness centers reducing relapse susceptibility
Physical vitality strengthens psychological resilience, so clinicians weave movement and diet into every treatment week. Certified trainers design low-impact routines that elevate dopamine without exhausting newcomers. Yoga, beach walks, and resistance circuits rebuild confidence in recovering bodies. Simultaneously, dietitians analyze micronutrient deficits common after prolonged substance misuse. Personalized meal plans stabilize blood sugar, reducing irritability that can mimic craving.
Educational cooking labs reveal practical hacks for busy schedules. Participants learn balanced snacks that fit glove compartments, blocking vending-machine binges during traffic jams. Supplements like omega-3 and magnesium receive evidence-based discussion rather than fad hype. Readers seeking deeper detail can explore nutrition guidance to curb relapse risk which outlines the biochemical rationale behind menu choices. As clients feel stronger, exercise and wholesome food transition from obligatory tasks to cherished rituals, making relapse far less attractive.
Individualized aftercare planning and sober living transition guidance in South Florida
Successful discharge begins on day one, not the final week. Case managers collaborate with clients to chart employment goals, continuing therapy frequency, and housing preferences. For many, structured sober living homes provide the ideal intermediate step between intensive outpatient programs and full independence. Staff vet residences for curfews, drug testing protocols, and community reputation, ensuring quality control.
Transportation logistics also receive attention. South Florida’s patchwork of public transit, ride-shares, and bike lanes can complicate meeting attendance. Therefore, planners map efficient routes to therapy, work, and grocery stores. Budget coaching prevents financial stress, a common relapse trigger. Finally, digital calendars schedule follow-up appointments six months out, embedding accountability. This meticulous orchestration converts uncertainty into an actionable roadmap that fosters confidence.
Relapse risk assessment tools and evidence-based coaching at treatment centers
Quantifying vulnerability lets clinicians intervene before danger peaks. Delray Beach IOP employs validated scales measuring stress tolerance, sleep quality, and social support. Results feed machine-learning dashboards that predict high-risk days with surprising accuracy. During review sessions, therapists translate data into plain language, then recommend targeted drills or medication adjustments. Clients appreciate the objectivity, which removes moral judgment from the equation.
When assessments reveal specialized needs, counselors may route clients toward specialized substance programs near Palm Beach for concentrated attention. Additional coaching sessions dissect relapse fantasies, turning abstract fears into solvable problems. Motivational interviewing keeps autonomy front and center, while skills labs rehearse exit strategies like “leave the barbecue early” or “text sponsor before office happy hour.” Step by step, evidence-based coaching transforms numbers on a chart into daily choices that protect sobriety.
Anchoring Resilience Sustaining Sobriety after Intensive Outpatient Care
Alumni networks and community resources for relapse prevention near you
The day discharge papers are signed does not mark the end of guidance; it marks a handoff. Alumni networks extend clinical momentum into daily life, offering mentors who understand coastal temptations. Group hikes, beach cleanups, and online forums keep connection fresh and purposeful. Whenever cravings whisper, someone who once sat in the same therapy circle answers the phone. Clients also use a directory to locate NA support groups locally for extra layers of peer accountability.
Formal alumni programming thrives because it is guided by the same evidence-based spirit that steers the IOP curriculum. Monthly workshops revisit coping tools and celebrate milestones with the enthusiasm of a championship locker room. Guest speakers share success stories that highlight realistic setbacks and the strategies that transformed them into stepping stones. Because growth never stalls, alumni can return for booster sessions whenever life throws unexpected curveballs. Prospective clients can learn about our recovery mission in South Florida to understand how this continuum forms a safety net.
Leveraging post-discharge check-ins and remote monitoring
Digital oversight bridges the vulnerable gap between structured therapy hours and unsupervised living. The Delray telehealth platform prompts daily mood check-ins that take less than one minute. Simple color-coded dashboards alert clinicians when stress or insomnia spikes above personalized thresholds. Rapid texts or video calls then deliver timely adjustments before cravings gather momentum. This immediate feedback loop strengthens the neural pathway that chooses support over secrecy.
Beyond daily logs, the program schedules graduated check-ins at one week, one month, and quarterly intervals. These appointments review sleep patterns, social stressors, and medication adherence with the precision of a flight engineer. When metrics show improvement, clinicians celebrate, reinforcing behavior change through positive neuroscience. If red flags flicker, the team reroutes clients into booster groups or suggests medication tweaks within hours. These refinements reflect our philosophy of continuously building winning recovery paths in Delray that adapt as life evolves.
Turning relapse risk into growth mindset lessons
Relapse risk loses power when framed as data rather than disaster. Counselors invite clients to dissect near-miss moments with the curiosity of a scientist. Together they chart triggers, emotions, and decisions on a whiteboard, transforming shame into strategy. Patterns emerge quickly, revealing specific early-recovery relapse vulnerabilities that can be addressed with targeted drills. Every insight becomes a blueprint for the next sober day, turning fear into forward motion.
Mindset coaching draws heavily from cognitive psychology, which shows that beliefs shape behavior more than circumstances. Facilitators teach language shifts, such as replacing “I ruined everything” with “I collected new information.” Clients practice these reframes until neurons wire optimism as the default emotional soundtrack. Research on neuroplasticity and understanding substance abuse challenges confirms that repeated positive framing rewrites reward pathways. With each cognitive pivot, relapse risk diminishes because the brain learns curiosity instead of catastrophizing.
Invitation to explore rehab in Delray Beach for enduring wellness
Sustained sobriety flourishes inside ecosystems that honor both science and soul. Delray Beach Intensive Outpatient Programs marries evidence-based protocols with the rejuvenating rhythm of ocean breezes. From first phone call to final graduation, every interaction aims to build trust and personalized mastery. Those considering help can review the easy admissions steps for Delray IOP and discover how seamless entry removes common barriers. A streamlined start frees mental energy for the real work: cultivating a life where relapse feels unnecessary and outdated.
Choosing a treatment center is ultimately a pledge to your future self. When that pledge is supported by licensed clinicians, resilient peers, and coastal serenity, the odds tilt favorably. Our team invites you to tour the facilities, meet alumni, and envision the possibilities that now wait within reach. Whether you battle alcohol, opiates, or co-occurring disorders, customized care plans await your signature. Take the next courageous step and allow Delray Beach IOP to anchor resilience that lasts long after therapy hours end.
 Frequently Asked Questions
Frequently Asked Questions
Question: How does Delray Beach IOP identify and manage triggers for relapse in intensive outpatient programs?
Answer: Every client receives a comprehensive relapse risk assessment during admission. We pair validated tools with one-on-one interviews to uncover personal and environmental triggers for relapse in intensive outpatient programs-everything from coastal nightlife to workplace stress. Those insights feed an individualized treatment plan that includes cravings management workshops near you, route-mapping to avoid high-risk zones, and cognitive-behavioral relapse management sessions that rehearse real-world refusal skills. By combining data, therapy, and practical scheduling, Delray Beach Intensive Outpatient Programs turns potential landmines into well-marked detours.
Question: What coping skills training for alcohol recovery and post-acute withdrawal symptom support can I expect at your Florida rehab center?
Answer: Coping skills training for alcohol recovery begins on day one. Clinicians teach urge-surfing, sensory grounding, and timed breathing protocols that calm neurochemical spikes common in post-acute withdrawal. We layer in mindfulness-based relapse prevention sessions, nutrition coaching that stabilizes blood sugar, and fitness programs that naturally boost dopamine. Digital journals track progress so therapists can fine-tune tactics in real time. This multidisciplinary toolkit minimizes discomfort, builds confidence, and dramatically reduces relapse risk at our Delray Beach IOP.
Question: In the recent blog Relapse Risk at Delray Beach Intensive Outpatient Programs, you highlighted telehealth monitoring-how does it protect clients from early-recovery relapse vulnerabilities?
Answer: Our secure telehealth platform prompts quick daily check-ins on mood, sleep, and stress. If a pattern hints at early-recovery relapse vulnerabilities-say, three nights of insomnia or an uptick in anxiety-the system flags your clinical team instantly. We respond with video coaching, medication adjustments, or emergency relapse intervention plans before cravings escalate. Families can also activate safety alerts if communication drops, creating a 24/7 safety net that stretches far beyond campus walls.
Question: How do individualized aftercare planning and sober living transition guidance in South Florida help lower relapse statistics in intensive outpatient settings?
Answer: Discharge planning starts the moment you arrive. Case managers collaborate with you to craft a step-by-step roadmap: curated sober living homes near the beach, ride-share routes to meetings, budget coaching to reduce financial stress, and scheduled alumni check-ins for accountability. Because every detail is mapped in advance, the chaotic gap between treatment centers and full independence disappears. National data show a one-third relapse rate after IOP, but our layered aftercare approach-complete with peer support in Delray Beach recovery programs-drops that figure dramatically for graduates who follow the plan.
Question: What role do family involvement and peer support networks play in reducing relapse risk at Delray Beach Intensive Outpatient Programs?
Answer: Family involvement and peer support networks create a protective buffer that lowers relapse risk long after therapy sessions end. At Delray Beach Intensive Outpatient Programs, loved ones join education groups that clarify relapse warning signs, boundary-setting, and supportive communication, so home environments reinforce recovery instead of triggering shame. In parallel, peer support networks pair newcomers with alumni mentors who understand coastal nightlife temptations, coordinate carpools to meetings, and keep accountability alive through check-in chains. This dual-layer support system reduces isolation, accelerates early intervention when cravings rise, and measurably improves outcomes for clients navigating intensive outpatient programs in Delray Beach.
